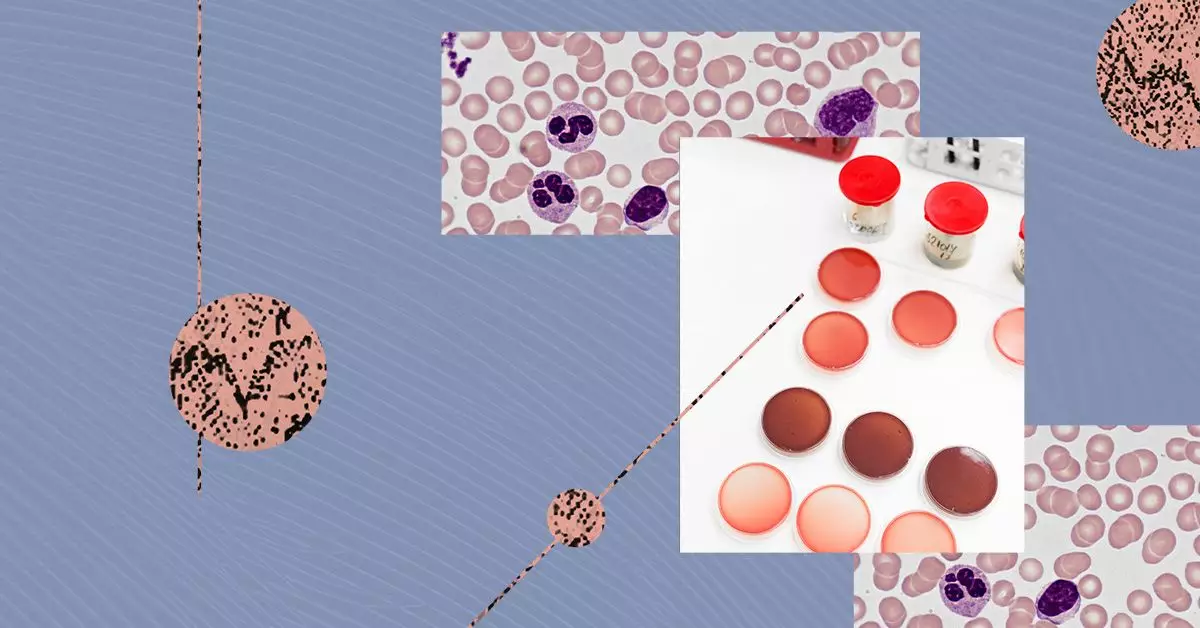
Multiple myeloma (MM) is a complex hematological malignancy characterized by the abnormal proliferation of plasma cells, a subtype of white blood cells vital for immune function. As this condition evolves, it manifests in several distinct ways, each requiring a tailored approach for diagnosis and treatment. This article will delve into the major variants of MM, their diagnostic significance, and how they interrelate with other plasma cell disorders.
At its core, multiple myeloma originates from the rapid and uncontrolled division of malignant plasma cells in the bone marrow. These atypical cells fail to carry out their normal function of producing antibodies necessary for immune defense, leading to a host of complications. The symptoms of MM arise from the crowding out of healthy blood cells, the production of abnormal proteins, and the degradation of bone and immune function.
It is pivotal for clinicians to differentiate between the various subtypes of MM to identify the optimal treatment strategies for patients. The main categories include typical myeloma, light chain multiple myeloma (LCMM), non-secretory myeloma (NSM), and IgM myeloma. Each subtype exhibits unique characteristics related to the type of immunoglobulin produced by the neoplastic plasma cells.
The most prevalent form, typical myeloma, can be further subdivided based on the type of heavy chains produced by the malignant cells. These chains, which class plasma cells into categories such as IgG, IgA, IgD, and IgE, determine the behavior and treatment response of the disease. Among these, IgG kappa myeloma stands out as the most common, followed closely by IgA myeloma.
Contrastingly, LCMM poses unique challenges both in diagnosis and management. Comprising approximately 15% of all MM cases, LCMM is characterized by the production of monoclonal light chains without significant levels of heavy chains. This variant tends to be more aggressive, leading to a poorer prognosis, highlighting the necessity for diligent monitoring and intervention.
On the rare end of the spectrum lies non-secretory myeloma, which accounts for only 1% to 5% of MM cases. The challenge with NSM is its subtlety; these patients often present minimal paraprotein levels, complicating both diagnosis and disease monitoring. The clinical implications of NSM remain underexplored, with limited data on its natural progression.
Among the distinct forms of MM, IgM myeloma represents a particularly rare subtype, contributing to less than 0.5% of cases. Its clinical features often overlap with Waldenstrom macroglobulinemia, creating diagnostic challenges that require careful consideration and differentiating investigative measures. The rarity of IgM myeloma may limit research and raise questions about optimal management strategies.
Apart from the primary subtypes of MM, several related disorders warrant attention due to their potential progression to active multiple myeloma. Smoldering multiple myeloma (SMM), classified as an early form of MM, is asymptomatic yet marked by elevated plasma cells and monoclonal proteins. While SMM rarely necessitates immediate intervention, some patients display a risk of rapid progression, placing them under closer clinical surveillance.
Solitary plasmacytoma, defined by isolated plasma cell tumors in soft tissues, may not fulfill the criteria for active MM but shows pronounced potential for developing into symptomatic cases. Treatment typically involves radiation therapy, and when managed effectively, patients can have favorable outcomes if no further lesions arise.
Another variant, monoclonal gammopathy of undetermined significance (MGUS), manifests as abnormal monoclonal protein without any significant complication, making it a non-cancerous condition. Nevertheless, MGUS carries a notable risk of evolving into more severe forms of plasma cell disorders, including MM. Regular monitoring and clinical vigilance are paramount for patients diagnosed with MGUS.
The landscape of multiple myeloma encompasses a range of variants, each with unique characteristics that inform treatment decisions and prognostic evaluations. Understanding these distinctions is vital for healthcare professionals in delivering patient-centered care and guiding appropriate monitoring strategies. Furthermore, recognizing related plasma cell disorders underscores the interconnected nature of hematological malignancies, providing a comprehensive approach to early detection and intervention. As research continues to evolve, it is imperative to remain abreast of updates in classification, treatment modalities, and patient management strategies to enhance outcomes for those affected by these aggressive conditions.