The human reproductive system is a complex and vital aspect of biology that plays a crucial role in the continuation of our species. Both the male and female reproductive systems have specialized structures that perform essential functions, including hormone production, sexual function, and the creation of offspring. This article delves into the intricacies of these systems, highlighting their components, life cycles, hormonal regulation, and common health issues that may arise.
The reproductive system comprises a series of internal and external organs that function together to facilitate reproduction, sexual activity, and hormonal balance. Each sex exhibits unique anatomical features and hormonal profiles that serve distinct reproductive goals. Understanding these functions helps demystify processes such as menstruation, pregnancy, and sexual health.
In exploring the female reproductive system, it is essential to recognize its dual components: the external and internal structures. The external organs, collectively referred to as the vulva, include the mons pubis, labia majora, labia minora, clitoris, and the urethra opening. These structures provide protective functions and play a significant role in sexual arousal and sensation.
Internally, the system encompasses the vagina, cervix, uterus, ovaries, and fallopian tubes. The vagina is a muscular canal that serves both as the birth canal and the passageway for menstrual flow. The cervix acts as a gateway between the uterus and the vagina, facilitating the entry of sperm while also allowing for menstrual blood to exit.
The ovaries are particularly noteworthy; they store immature eggs and produce hormones like estrogen and progesterone, which regulate various functions related to the menstrual cycle and pregnancy. Each month, during ovulation, a maturing egg is released and transported through the fallopian tubes, where fertilization may occur if sperm is present.
The Menstrual Cycle: A Monthly Rhythm
The menstrual cycle is a remarkable physiological process that prepares the female body for potential pregnancy. It typically spans around 28 days and is driven by hormonal fluctuations. As estrogen and progesterone levels rise and fall, various changes occur, including the thickening of the uterine lining and the maturation of eggs.
Menstruation occurs when an egg is not fertilized, leading to the shedding of the uterine lining. This monthly cycle is vital for women’s reproductive health and can influence physical and emotional well-being. Imbalances in this cycle can lead to conditions such as polycystic ovary syndrome (PCOS) or amenorrhea, both of which may necessitate medical intervention.
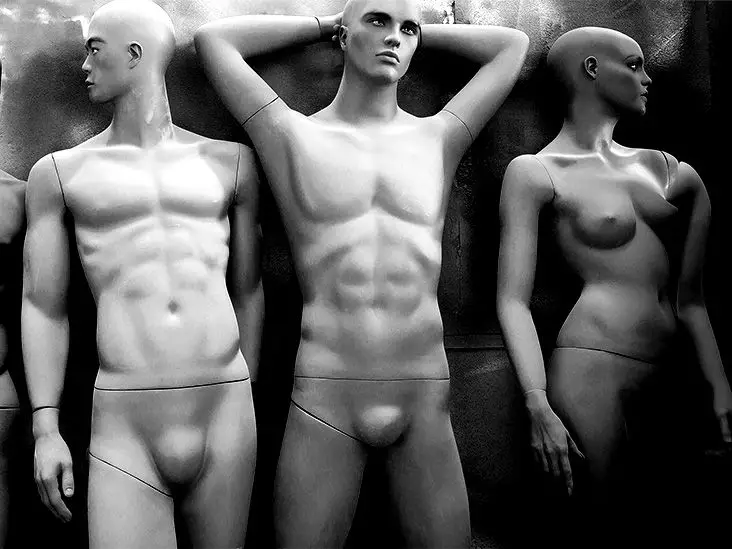
Contrasting with the female system, the male reproductive system is designed primarily for the production and delivery of sperm. Key components include the penis, testicles, epididymis, prostate, seminal vesicles, and the vas deferens. The penis serves as the conduit for urine and semen, while the testicles are responsible for sperm production.
Within the testicles, sperm matures and gains mobility in the epididymis, a coiled structure where it is stored until ejaculation. The prostate and seminal vesicles produce seminal fluid, which nourishes sperm and aids in its transportation during ejaculation. Together, these components work harmoniously to ensure successful reproduction.
Hormones are fundamental to the proper functioning of both male and female reproductive systems. In females, follicle-stimulating hormone (FSH) and luteinizing hormone (LH) regulate the menstrual cycle by stimulating ovulation and influencing estrogen and progesterone production. In males, LH and FSH play comparable roles in testosterone production and sperm maturation.
These hormones not only control reproductive functions but also contribute to secondary sexual characteristics such as breast development, body hair growth, and changes in voice. Hormonal imbalances can lead to reproductive challenges, including infertility and other health issues, making awareness of these interactions crucial.
It’s also important to address intersex individuals whose reproductive anatomy does not align strictly with traditional definitions of male or female. Intersex conditions can vary significantly, leading to diverse anatomical presentations. Recognizing and understanding these variations challenge the binary notion of gender and call for more inclusive perspectives in reproductive health discussions.
Despite the remarkable design of the reproductive systems, various health issues can arise, ranging from infections to hormonal disorders and structural abnormalities. In females, conditions such as endometriosis, uterine fibroids, and polycystic ovary syndrome are common. Males might face issues like erectile dysfunction or infertility related to sperm production problems.
A proactive approach to reproductive health should include regular check-ups, awareness of symptoms, and open communication with healthcare providers. Gynecologists assist with female reproductive health, while urologists specialize in male reproductive concerns. Additionally, mental health support is vital as reproductive health can profoundly impact emotional well-being.
An understanding of the reproductive system is essential not only for those looking to conceive but also for anyone interested in maintaining overall health. By fostering awareness around the complexities of both male and female reproductive systems, we can promote healthier practices, encourage timely medical interventions, and ultimately empower individuals to take control of their reproductive health. Through education and communication, the mysteries surrounding reproduction can transform from a source of confusion into a foundation of knowledge.